The Centers for Disease Control and Prevention (CDC) recently released estimates of drug overdose deaths for May 2020 through April 2021 that show a 27 percent increase relative to the previous 12 months. This reverses the trend observed between 2017 and 2019, when increases in overdose deaths stalled. In light of accelerating overdose deaths, it is important to reflect on the role the COVID-19 pandemic may have played in stemming progress, and to consider whether new approaches are needed in the fight against the opioid epidemic.
Drug overdose deaths climbed in 2020 and 2021 after plateauing over the previous three years.
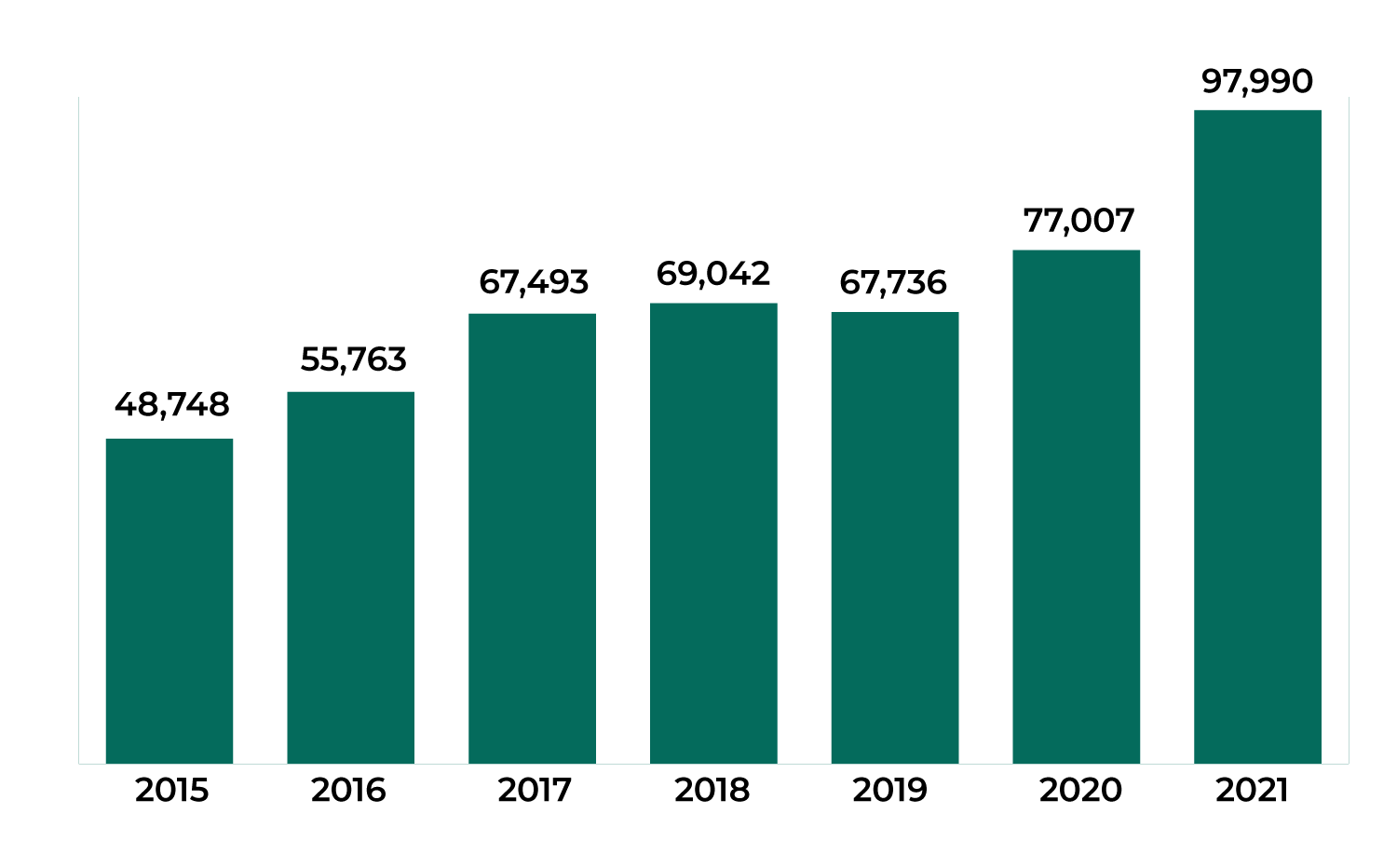
Source: Mathematica analysis of CDC vital statistics data available here.
Stemming the opioid epidemic generally focuses on three areas: 1) prevention, 2) effective treatment services and recovery supports, and 3) drug supply reduction. There has been progress and some setbacks in each of these areas.
Prevention programs may be working for young adults, but older adults account for most opioid disorders.
Mathematica recently analyzed progress in preventing substance use disorders (SUDs) between 2015 and 2018, a period marked by substantial federal, state, and local efforts to stem the opioid epidemic. Perhaps because of such efforts, the percentage of young adults ages 18–25 with an opioid use disorder declined 40 percent and those misusing pain relievers declined 42 percent. From 2017 to 2018, heroin use disorders among 18–25-year-olds declined 40 percent. In contrast to the improvements for young adults, the changes in other age groups were not statistically significant. Although the progress in preventing disorders among young adults is commendable, the lack of progress for adults ages 26 or older is troublesome, since they represent 79 percent of all people with an opioid use disorder. New estimates for 2020 suggest potential declines in prevalence for adolescents and young adults, but consistent prevalence for adults 26 or older during the COVID-19 pandemic.
Opioid use disorders declined among adolescents and young adults, but not adults 26 or older.
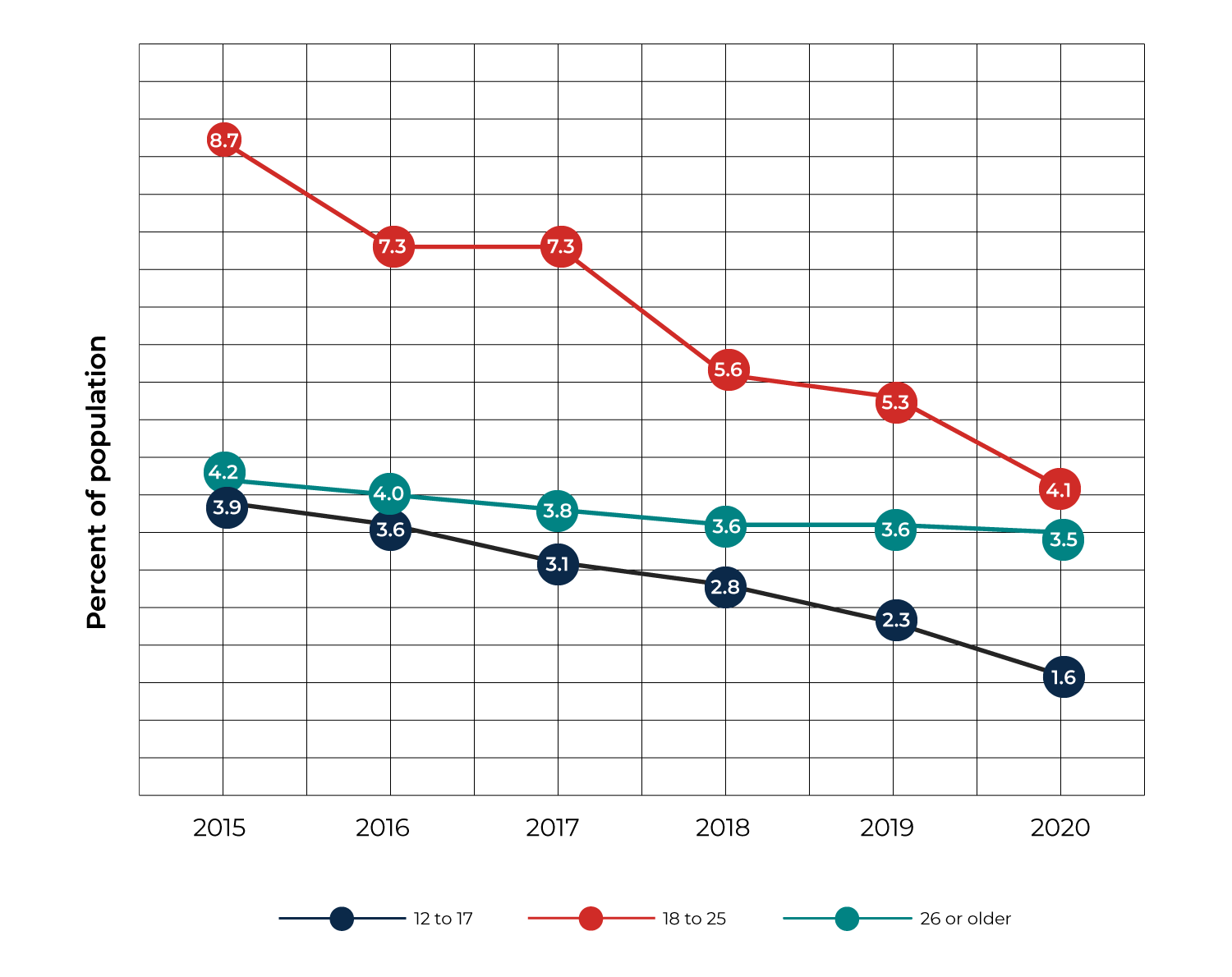
Source: Substance Abuse and Mental Health Services Administration. “Key Substance Use and Mental Health Indicators in the United States: Results from the 2020 National Survey On Drug Use and Health.” U.S. Department of Health and Human Services Publication #PEP21-07-01-003, NSDUH Series H-56. Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration, 2021. Retrieved from https://www.samhsa.gov/data/.
Notes: Caution should be used when comparing estimates for 2020 to earlier years because of methodological changes for 2020. See the 2020 National Survey on Drug Use and Health: Methodological Summary and Definitions for details.
Treatment for substance use disorder has been on the rise but declined during the COVID-19 pandemic.
Recent Mathematica studies have assessed trends in access to SUD treatment and the quality of treatment provided. Analysis of trends in SUD treatment suggests increased access to SUD treatment in private doctors’ offices and to intensive and regular outpatient treatment in specialty SUD treatment facilities. The analysis also indicates a substantial (20.5 percent) increase in the rate of medication-assisted treatment (MAT) use between 2015 and 2017 and potential increases in the duration of care for those who receive SUD treatment. These improvements are likely to have positive ramifications for long-term outcomes, as MAT is a highly effective and underused treatment approach. Guidelines and research on MAT support long-term treatment because the risk of relapse is high when MAT is discontinued.
However, despite these improvements, the rate of any treatment use for individuals with opioid use disorder was only 19.7 percent in 2018, showing there was substantial unmet need for treatment before the COVID-19 pandemic. Meanwhile, recently published data indicates a 13 percent decline in SUD treatment for Medicaid and Children’s Health Insurance Plan beneficiaries during the COVID-19 pandemic from March to October 2020, compared with the same months in 2019. In addition, telehealth services have represented a greater share of SUD treatment since the pandemic began, and there is a limited understanding of what this shift implies for care quality.
The quality of treatment programs improved before and during the COVID-19 pandemic.
Other recent Mathematica studies provide insight into trends in the quality of SUD treatment. For example, one study looked at changes in staffing at opioid treatment programs between 2011 and 2016 and found that in this period, staffing levels per client served increased substantially across all staff types, including medical and counseling staff. Although there is limited research on the relationship between staffing and care quality, increases in medical and pharmacy staff are likely associated with increased provision of MAT—which is associated with improved patient outcomes such as increased retention in treatment and reductions in illicit drug use and overdose deaths. Another study reviewed trends in treatment offerings at SUD treatment facilities during the COVID-19 pandemic and found that the percentage of clients at inpatient facilities receiving buprenorphine more than doubled from 19 to 48 percent. This increase has the potential to improve patient outcomes because providing buprenorphine during inpatient care reduces mortality and improves retention in outpatient treatment.
Declines in opioid prescribing were eclipsed by a flood of highly potent fentanyl.
Our assessment of progress in reducing the availability of drugs highlights the complexity of controlling access to potentially harmful drugs. Acknowledging the role that prescription opioids played in creating the opioid epidemic, the CDC, state governments, healthcare providers, and insurers implemented policies and guidelines to reduce opioid prescribing. Between 2012 and 2020, opioid prescriptions declined 44 percent, representing a substantial reduction of availability. Unfortunately, overdose deaths did not decline in parallel to reductions in prescription opioids. Instead, fentanyl, alone or in combination with other drugs including methamphetamine and cocaine, increasingly flooded the illicit drug market. Extremely potent in very small quantities, illicit fentanyl is easily trafficked, highly variable in dosage, and invisible when mixed with other substances, putting both intentional and unintentional users at increased risk of overdose. With about 90 percent of illicit drugs entering the United States from Mexico, increased border security associated with the COVID-19 pandemic initially reduced illegal drug traffic, but cartels have adapted and developed new trafficking approaches. Further, seizure of fentanyl by United States Customs and Border Protection increased 134 percent between federal fiscal years 2020 and 2021, but these efforts to address supply have not stemmed the increase in overdose deaths.
Overall, in each of the three focus areas, there has been some success in addressing the opioid epidemic. However, the COVID-19 pandemic was associated with substantial setbacks—SUD treatment declined, and overdose deaths increased. In the face of these setbacks, maintaining existing strategies is not enough. Addressing this challenge will require focused effort in various areas.
Address declines in treatment use associated with the COVID-19 pandemic through evidence-based interventions and reducing barriers to treatment access.
The decline in SUD treatment use associated with the COVID-19 pandemic was primarily related to reductions in new admissions. Patients may have been less likely to seek treatment because of concerns about becoming infected with COVID-19 or less able to access treatment due to reduced facility capacity during the pandemic. Ensuring patients have access to vaccines and facilities have adequate resources and protocols in place to reduce the risk of transmission may stem patient concerns about this risk and allow facilities to return to normal capacity. However, the primary reasons reported by individuals with SUDs for not receiving treatment were similar in 2020, the first year of the COVID-19 pandemic, to those from prior years. Among individuals meeting symptomatic criteria for an SUD, but not receiving SUD treatment, 97.5 percent reported they did not feel they needed treatment. Among the 2.5 percent who felt they needed treatment, but did not receive it, 19.1 percent noted concerns about cost, 14.4 percent had concerns about finding a program with the type of treatment they wanted, and 11.9 percent were concerned about the stigma associated with treatment. If these individuals are facing social, financial, legal, or health problems because of their alcohol or drug use, they can benefit from educational programs or brief interventions that identify risks of substance use and potential approaches to reducing substance use that align with their values and goals. These interventions can be provided in emergency departments, doctors’ offices, or criminal justice and hospital inpatient settings. Adults who are 26 and older should be a particular focus. Addressing cost concerns will require ensuring treatment is available at minimal cost to patients and that patients are aware of the low cost. Providing a continuum of services in all localities would address patients’ inability to find a program that offered the type of treatment they want. Finally, reducing the stigma associated with receiving treatment might start with ensuring the health and social service professionals that individuals with SUDs encounter have training on how to interact with them in a compassionate and caring manner and employing the most efficacious treatment and motivation enhancing approaches.
Identify the strengths and limitations of telehealth treatment. Treatment via telehealth expanded rapidly during the COVID-19 pandemic. While counseling and medication management services are likely to continue to be provided via telehealth, it is clear this has limitations for some patients and service types. Some providers expressed reluctance to initiate treatment via telehealth. Others noted that some patients with low income may lack reliable access to the necessary technology, while other patients are distracted during telehealth treatment or lack needed privacy in their home. Finally, collecting clinical data, such as urine screens, is more difficult or impossible via telehealth. Understanding how telehealth can be effectively integrated into the existing system of care while preserving or increasing care quality is critical and will require additional research.
Ensure access to integrated treatment for individuals with co-occurring mental health disorder and a SUD. Because mental health disorders and SUDs can contribute to the development of and exacerbate the other, it is important for SUD treatment providers to screen for a mental health disorder and provide integrated care when both are present. In 2020, 45 percent of individuals with a SUD had a co-occurring mental health disorder. Co-occurring disorders are a recognized factor in SUD treatment, with 71 percent of treatment facilities reporting they provided mental health services in 2020. However, the COVID-19 pandemic may have increased the importance of addressing co-occurring disorders, as 18.3 percent of adults reported that the COVID-19 pandemic negatively affected their mental health “quite a bit or a lot.”
Examine the relationship between staffing patterns and service offerings and the quality of treatment. Staff interactions and the services patients receive are a key component of successful SUD treatment. Staffing patterns and service offerings vary substantially across facilities providing the same level of care. These differences may stem from differences in the needs of the patients each facility serves, but they are not well understood. A number of models, including the Hub-and-Spoke model, Nurse Care Manager model, Project ECHO model, and telemedicine have increased access to SUD treatment in response to the opioid epidemic and the COVID-19 pandemic. Research assessing the implications of differences in models, staffing patterns, and service offerings for patient outcomes would provide a foundation for directing supplemental SUD treatment resources most effectively.
Focus on harm reduction. Focusing on the supply network may temporarily reduce the flow of fentanyl into the United States or into particular drug markets; however, fentanyl can be produced cheaply and is potent in small amounts. Therefore, permanently disrupting supply is challenging. Stemming overdose deaths is likely to require implementation of harm reduction strategies. These strategies include the following measures:
- Focusing law enforcement activities on dealers who supply products most likely to result in overdose and providing first responders with naloxone
- Providing individuals with opioid use disorder access to MAT; currently, less than 20 percent of individuals with opioid use disorder receive MAT, and those with prescriptions can struggle to fill them since only one in five pharmacies carries buprenorphine
- Educating individuals who use drugs on how to reduce their risk of overdose by using illegal drugs more slowly, doing so-called test shots to gauge potency, identifying and abstaining from use of counterfeit pills, using clean syringes, and carrying naloxone
- Providing access to needle exchanges and adulterant screening supplies (such as fentanyl test strips)
We cannot lose sight of the recent progress and let the recent setbacks become new trends. Over the last two years, if we had simply maintained the 2019 levels, we would have avoided nearly 40,000 drug overdose deaths. The combination of challenges associated with the COVID-19 pandemic and the influx of highly potent fentanyl mean we are unlikely to return to pre-pandemic levels without additional investment in promising strategies.



