The supply of health care providers for patients living with HIV is not keeping pace with the growth in demand for their services, according to the first large-scale study of America’s HIV clinician workforce.
Over 1 million people in the United States live with HIV or AIDS, and another 50,000 become infected each year. In the first national survey to examine the HIV clinician workforce, Mathematica Policy Research and its partner, the Lewin Group, identified the number, type, and practice patterns of health care providers (including physicians, nurse practitioners, and physician assistants) who manage care for patients living with HIV or AIDS in the United States.
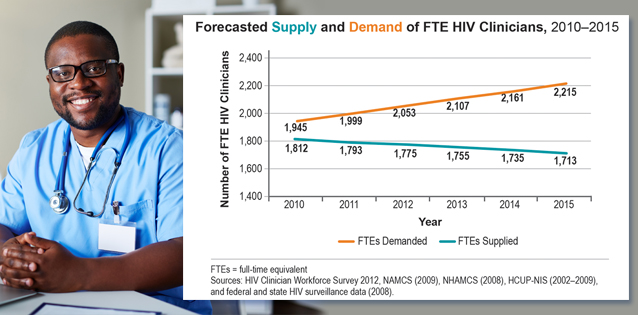
First published in the August issue of HIV Specialist, the quarterly magazine of the American Academy of HIV Medicine, an article by Mathematica researchers Boyd Gilman and Ellen Bouchery reported that the number of full-time equivalent (FTE) HIV providers was expected to decline over 5 percent nationally from 2010 to 2015, while the demand for their services would increase almost 14 percent. The report estimates that there was a shortage of 133 FTE HIV clinicians in 2010 (representing roughly 7 percent of actual supply), which would grow to a shortage of 502 clinicians in 2015 (representing nearly 30 percent of actual supply).
“We have reason to believe this trend is continuing and will likely have long-term adverse consequences for public health if not addressed,” noted Gilman. “Unlike other medical specialties, such as family medicine, general practice, and infectious disease, HIV care lacks an established credentialing requirement, and patients seek care from a variety of providers. This study offers important insights into how HIV clinicians practice and how the HIV workforce might be enhanced in the future.”
Additional findings include:
- The shortage of HIV providers comes as new people become infected and those living with the disease survive longer. In addition, the number of providers entering the HIV workforce is not sufficient to fill the gap left by those leaving the profession. Demographic shifts in the HIV workforce are also leading to a decrease in the average number of hours providers work each week.
- The 2010 Affordable Care Act, implemented after the study was conducted, will contribute to the growing gap in care as more people living with HIV gain insurance coverage and seek and remain in care. Efforts to expand testing and improve linkages, engagement, and retention in care will also increase demand for services.
- Many providers treat a small number of HIV patients and do not manage the HIV treatment of these patients on an ongoing basis. Training or professional support, such as helping primary care providers to co-manage care with HIV specialists, may help expand the workforce in the future.
- Nurse practitioners and physician assistants are an important component of the HIV workforce. Effective workforce strategies will need to be tailored to differences in training and scope of practice across the range of HIV practitioners.
The study, which Mathematica conducted for the Health Resources and Services Administration of the U.S. Department of Health and Human Services, assessed whether the supply of providers would be sufficient to address the goals of the National HIV/AIDS Strategy, launched by the White House Office of National AIDS Policy in 2010.
Using a national, all-payer claims database, the study identified 4,937 clinicians who provided care to at least 10 patients with HIV in 2010, and adjusted the number for new entrants minus losses from retirement and mortality through 2015. To estimate the total number of visits supplied, the authors multiplied the supply of HIV clinicians by survey-based estimates of the average number of hours worked per year, the proportion of time spent in HIV care, and the number of visits provided per hour. The authors calculated the number of individuals diagnosed with HIV in each year as the number of individuals diagnosed with HIV in the prior year plus newly diagnosed cases minus mortality, based on Centers for Disease Control and state and local surveillance data. They multiplied average utilization rates per diagnosed person by the forecasted number of diagnosed cases in each age and gender category to obtain the total number of HIV visits demanded in each forecasted year. The authors converted forecasted visits supplied and demanded to FTE clinician values based on the average number of HIV-related visits supplied per full-time clinician in the base year, and projected the numbers from 2011 through 2015.
About HIV Specialist
HIV Specialist is published by the American Academy of HIV Medicine, a professional organization that supports the HIV practitioners and promotes accessible, quality care for all Americans living with HIV disease. Its membership of HIV practitioners and credentialed providers gives direct care to the majority of HIV patients in the United States.