For more than a century, public health officials have used contact tracing and case investigation as the leading tools to manage the spread of disease. This is no different in the case of the COVID-19 pandemic. Contact tracers identify people who have been exposed to COVID-19 and ask them to quarantine. This tactic not only helps manage the spread of disease, but also provides valuable information about the places and environments where transmission happens. It’s only effective, however, if people are willing to share information with contact tracers, which is why trust between the contact tracers and people who have been exposed to the virus is an essential factor in making a contact tracing program work.
The evidence suggests that contact tracers can more effectively gain that trust when they share similar backgrounds with the people they’re calling. For example, people might be more likely to respond to questions and provide honest answers if the contact tracer speaks the same language they do. This is a particularly important way to improve the efficiency of contact tracing. Therefore, it is a good idea to hire from the community when building a contact tracing workforce, and to intentionally recruit contact tracers whose backgrounds are similar to the backgrounds of people in the community.
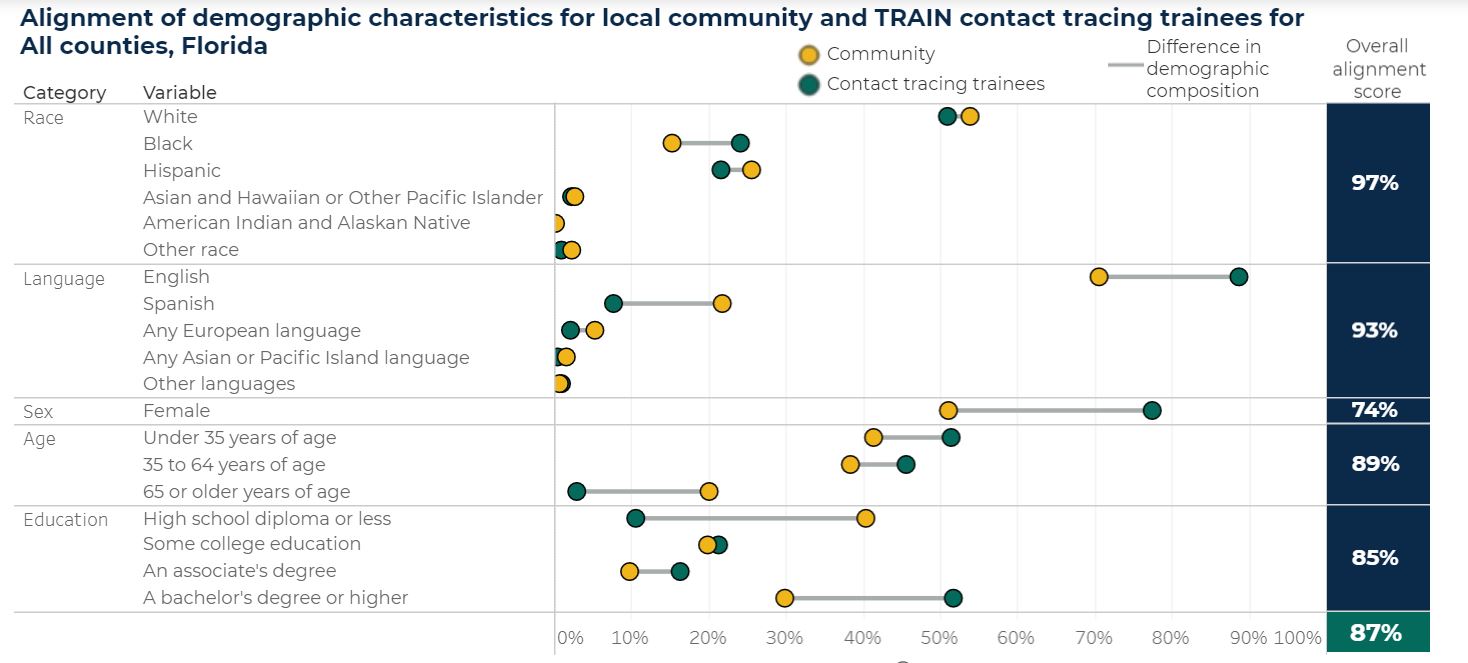
To help states, counties, and others develop strategies to better understand their communities’ contact tracing needs, staff at Mathematica and the Public Health Foundation (PHF) have developed an interactive dashboard to present key demographic characteristics of trainees who received training in contact tracing through the TRAIN Learning Network as well as the communities they serve. In particular, this effort demonstrates how such a dashboard could help the contact tracing workforce planning team to initiate a discussion about potential needs from the community and to develop the most effective contact tracing workforce possible. The dashboard would be especially helpful if comprehensive information—including contact tracing workforce data from TRAIN as well as other sources—became available. For example, 21.8 percent of the Florida residents speak Spanish at home, indicating a high need for Spanish-speaking contact tracers. According to the dashboard, 7.7 percent of the contact tracing trainees who chose to receive their contact tracing training through the TRAIN Learning Network speak Spanish as their first language, as of February 17, 2021 (Figure 1). Similar language gaps can be identified in states and counties across the country.
For data on local contact tracing trainees, we relied on information about people who received training through the TRAIN Learning Network, a service of the Public Health Foundation. The TRAIN Learning Network provides a robust clearinghouse of learning opportunities available for health professionals, and has 34,771 contact tracing trainees as of February 17, 2021. We should note, however, that other organizations provide contact tracing training as well. As of December 2020, the size of the nation’s COVID-19 contact tracing workforce was estimated to be higher than 70,000. The dashboard discussed in this blog only presents characteristics of contact tracing trainees who received training from the TRAIN Learning Network, which may not be representative of the total contact tracing workforce in the U.S.
Given the limits of TRAIN’s data, we can’t be certain how to interpret these kinds of gaps, but they could be generating important insights about where to direct limited resources to support ongoing contact tracing training. One likely reason why fewer contact tracing trainees in our dashboard speak Spanish as a first language is that the TRAIN platform is in English, so Spanish-speaking trainees might naturally seek out training from another source. In other words, the apparent gap in native Spanish speakers between the TRAIN contact tracing trainees and the communities they serve could be a quirk of the TRAIN platform and dataset, or it could reflect a broader trend in the contact tracing workforce. In either case, however, the dashboard’s data on what language the residents in the community speak can inform where demand is greatest for contact tracers who speak Spanish. (Figure 1).
The need for and alignment of backgrounds between contact tracers and community members will, of course, vary by locality. For example, only 11.2 percent of the Alaska residents are 65 or older, whereas Florida has a much higher proportion of older residents (Figure 1). Although it is unnecessary to match the contact tracer’s age to the age of most community members, contact tracing for older people presents unique challenges. They may have limited access to news and public health updates. They are more likely to experience mood disorders, cognitive impairments, or other mental health issues, such as Alzheimer’s. If they’re living alone, they may also lack social and emotional support. Insights from the dashboard about the age distribution in a community could inform states and counties about the backgrounds and skills their contact tracers will need to be most effective. To better serve residents who are 65 or older, states and counties might want to consider providing relevant communication training and strategies to contact tracers. They might also want to recruit contact tracers who have prior experience working with people in that age group.
Overall, building a contact tracing workforce whose demographic profile is well aligned with the local community is particularly important for states and counties with large communities of color and residents older than age 65. People in these groups often have higher rates of infection. Many are part of the essential workforce that cannot work from home and face economic and logistical hurdles that make it difficult to quarantine for two weeks.
Figure 1. Alignment chart of the dashboard as of February 17, 2021
Sources:
Public Health Foundation; The American Community Survey, U.S. Census Bureau; Geocoding and surname analysis to impute missing race/ethnicity BISG and Surgeo
Note: Demographic information is self-reported by contact tracing trainees. Some trainees did not report their demographics.
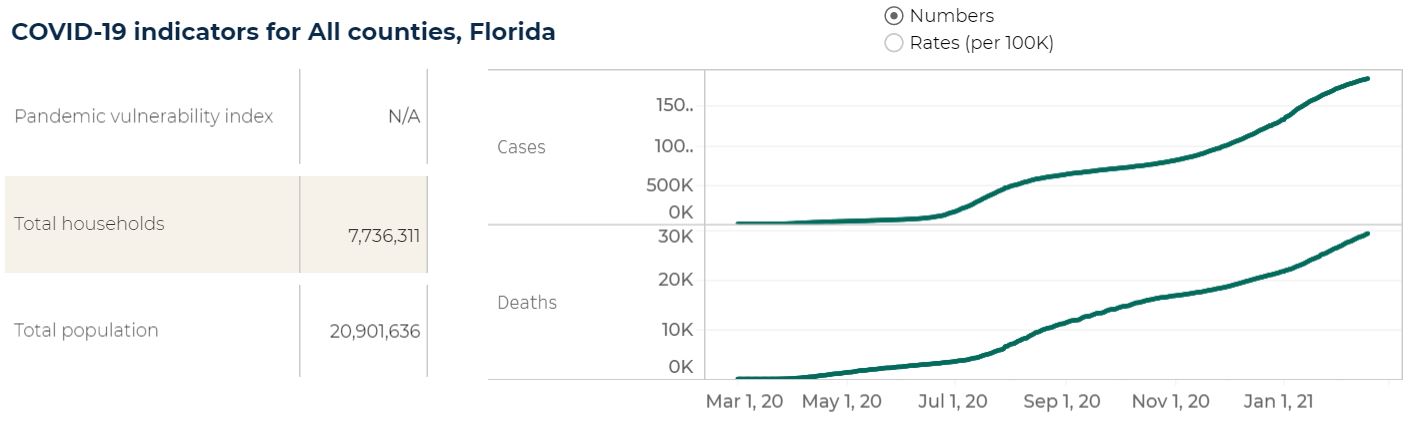
The need for contact tracing will not stop with the vaccine rollout. Over the winter holidays, cases rose (Figure 2). Even though Americans are starting to be vaccinated against COVID-19, it will be many months before the vaccine reaches the general population, and the take-up rate might be low in communities with inadequate access, or if a high proportion of residents choose to forgo the vaccine. For those reasons, throughout 2021 and possibly even later, it will remain important to continuously implement and refine COVID-19 contact tracing programs to effectively reach and gain the trust of their communities.
Figure 2. COVID-19 indicators of the dashboard as of February 17, 2021
The TRAIN Learning Network brings together thousands of partners and works closely with the health departments in 26 states. If data from all sources that provide contact tracing training were included in this dashboard, we could assess potential gaps in the current contact tracing workforce nationwide and help states, counties, and others build a contact tracing workforce that meets the needs of their communities.
We welcome partnership opportunities to update the dashboard with contact tracing workforce data from other sources. Please contact us at CTINFO@mathematica-mpr.com if you would like your information about the contact tracing workforce to be included in the dashboard.



