The latest results from Mathematica’s evaluation of Comprehensive Primary Care Plus (CPC+) show reductions in emergency department (ED) visits and acute hospitalizations after four years, though overall savings to Medicare were offset by increases in expenditures on other services, such as physician services and hospice.
CPC+, a national multipayer primary care improvement model developed by the Centers for Medicare & Medicaid Services (CMS), was the largest and most ambitious primary care and delivery reform ever tested in the United States. CMS launched CPC+ in 2017 and it ran through December 2021, supporting 3,070 primary care practices’ efforts to improve the care they provide to over 17 million patients. This report is on the fourth year of Mathematica’s independent five-year evaluation.
“Practices participating in CPC+ have been able to reduce emergency department visits and hospitalizations by increasing patient access to care and providing more focused care management,” said Sean Orzol, principal researcher at Mathematica. “Yet despite lower hospital expenditures, total Medicare spending hasn’t gone down. Rather, it has stayed the same due to increases in other costs such as greater hospice use and more physician outpatient services.”
The evaluation also found that participating practices cited care management fees as the most useful type of CPC+ payment support they received. Practices primarily used these fees to fund the salaries of care managers, behavioral health care providers, and other staff to improve care delivery.
The annual increase in the number of sites with on-site behavioral health specialists was particularly valuable over the fourth year as the COVID-19 pandemic increased mental health care demand during a very challenging time to secure services.
Percentage of practices that reported having a full- or part-time behavioral health specialist at the practice site, by track and program year
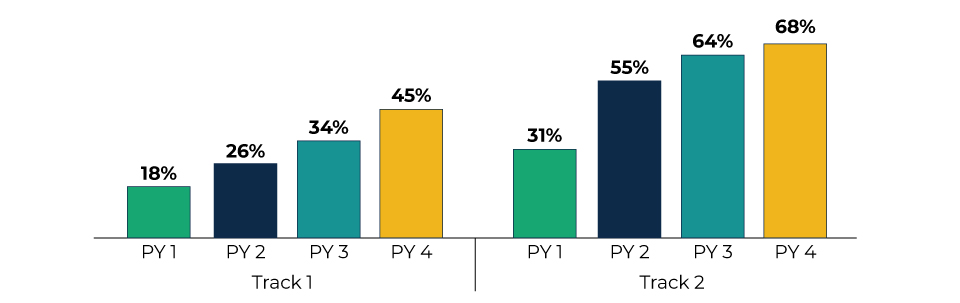
Source: Mathematica's analysis of data from the independent evaluation’s CPC+ Practice Surveys.
Note: N = 1,119 Track 1 practices and 1,337 Track 2 practices. Not all practices responded to the question each year. The percentage of missing responses each year was less than 1 percent. Compared to Track 1, Track 2 practices have more advanced care delivery requirements, receive additional financial support, and are required to gradually shift from a fee-for-service (FFS) approach toward population-based payment, all intended to better support patients with complex needs.
PY = Program Year.
Along with the report is a Findings at a Glance that summarizes key findings from the fourth year of the evaluation. Additional findings of note include:
- Practices’ ability to work on CPC+ care delivery requirements was hindered by the COVID-19 pandemic, but a range of supports (such as care managers) and temporary changes in payment policies (such as Medicare fee-for-service payment for telehealth) helped practices continue to fund their COVID-19 work.
- Between 2016 and 2020, long-term opioid use and potential overuse decreased among CPC+ beneficiaries.
- Practices continued to be satisfied with their decision to join CPC+ and reported that it improved the quality of patient care, though they thought CPC+ requirements—especially for financial reporting—were burdensome.
Mathematica is independently evaluating the implementation and impacts of CPC+ to determine if the model achieves its goal of increasing access to primary care, and ultimately achieving better health outcomes at a lower cost. The evaluation also examines whether CPC+ enhances primary care physicians’ experiences.
This evaluation presents findings from CPC+ in 2020, the fourth year of the five-year evaluation. It shows a growing effect on many, but not all, of the goals for primary care transformation among the participating practices.
Check out additional findings and insights about CPC+ here. Findings from the full evaluation, including its final year, will be forthcoming next year.
Contact
-
Christal Stone Valenzano
cstone@mathematica-mpr.com
202-250-3520


