Carol Irvin’s 30-year career has focused on using data to assess policies and programs related to health care access, particularly for vulnerable populations.
She has extensive experience managing work to support Federal Medicaid and CHIP operations and evaluating programs that extend coverage or transform health care services for people of all ages and with a wide range of chronic conditions and disabilities.
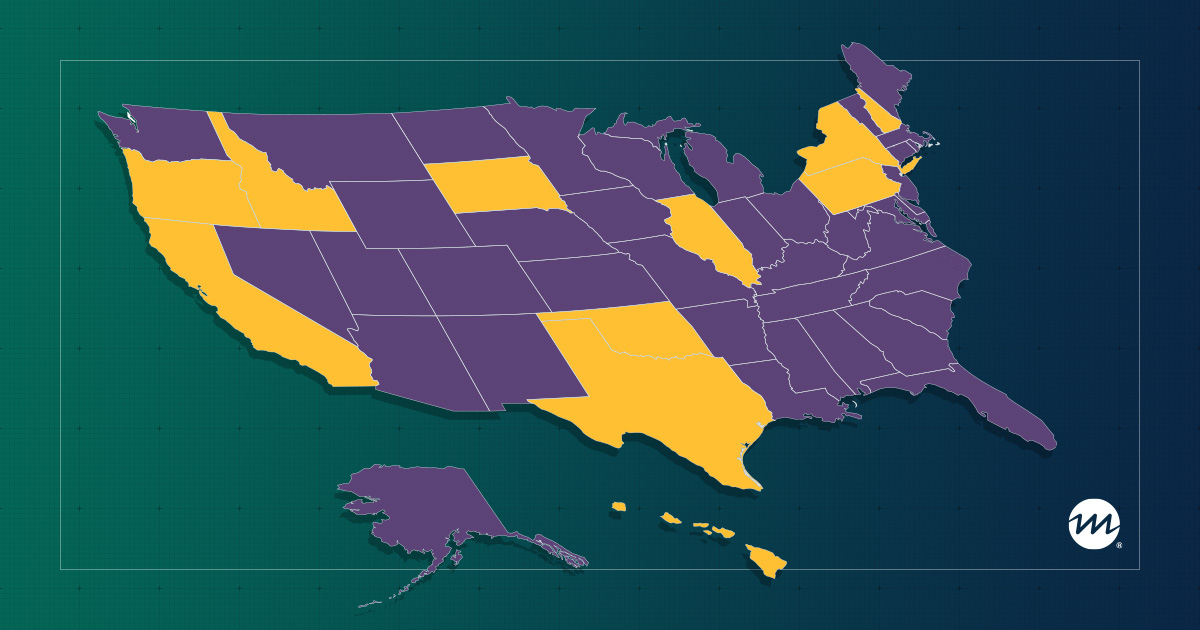
Irvin currently directs Mathematica’s Medicaid and CHIP (Children’s Health Insurance Program) Business Information System Business Analytics and Data Quality Development contract. This project supports the national Medicaid and CHIP data systems, the Transformed Medicaid Statistical Information System (T-MSIS) and Performance Indicator data, which the Center for Medicaid and CHIP Services uses to enhance its ability to make data-driven decisions about Medicaid and CHIP policies and programs. Under this contract, Mathematica monitors the quality of state T-MSIS data submissions, providing technical assistance to help states improve their T-MSIS data; designs and produces research versions of the T-MSIS data; conducts stakeholder engagement and training activities; produces reports and other analytic products that respond to stakeholder needs, such as the Data Quality (DQ) Atlas; and provides subject matter expertise on data design and management. This contract also provides technical support for the Medicaid and CHIP Accountability Scorecard, a Centers for Medicare & Medicaid Services initiative to improve the performance of Medicaid and CHIP programs.
Her program evaluation work includes leading Mathematica’s national evaluation of the Money Follows the Person demonstration, a Medicaid program that seeks to help states develop and strengthen approaches to transitioning people from institutional to community-based care. She also directed Mathematica’s initial evaluation of Section 1115 Medicaid demonstration programs. Her state-level evaluation work includes leading an evaluation of Oregon’s Medicaid 1115 demonstration that sought to transform how Medicaid services are managed and delivered. She also conducted an evaluation of the Healthy Indiana Plan, an innovative program that provided a high-deductible health plan for uninsured, working age Hoosiers. In other work, she contributes to studies of behavioral health services and home- and community-based services for the Assistant Secretary for Planning and Evaluation, conducts quality assurance reviews of Mathematica analyses of long-term services and supports, and evaluations of statewide plans to improve services of children with autism spectrum disorders.
Irvin, who publishes in peer-reviewed journals including Pediatrics and Psychiatric Services, presents at professional meetings such as the Medicaid Enterprise Systems Conference, AcademyHealth’s Annual Research Meeting, and the American Public Health Association annual meeting. She holds a Ph.D. in economics from the University of Wisconsin–Madison.