Transforming Rural Health Through Innovation and Evidence
Across the country, rural communities are working to keep essential healthcare within reach. Hospital closures, workforce shortages, and aging infrastructure threaten access to preventive, specialty, and emergency services. Through initiatives like the Rural Health Transformation Program, Mathematica partners with state, local, and federal leaders to design and scale solutions that strengthen financing, expand access, and improve the quality of rural care.
Achieving Rural Health Transformation
The Centers for Medicare & Medicaid Services’ Rural Health Transformation Program (RHTP) offers state leaders an opportunity to secure federal funding to redesign care delivery, strengthen access, and improve outcomes for rural communities.
Mathematica—backed by decades of experience working closely with CMS—provides comprehensive support throughout every stage of the transformation process. From developing strategies to delivering technical assistance and program design expertise, we work hand in hand with states to navigate program requirements, forge partnerships, and build scalable solutions grounded in data, evidence, and local needs and priorities.
Unlocking Funding from the Rural Health Transformation Program
Rural hospitals and providers are lifelines for their communities, but thin margins and workforce shortages threaten their future. To address these challenges, state leaders are designing new strategies for sustainable rural health care delivery and pursuing support for these efforts through the Rural Health Transformation Program.
Mathematica’s new data tool can strengthen states’ planning process by showing how rural factors—such as population size and uncompensated care—will shape award amounts. This information can help state leaders sharpen their strategies and ground planning and policy conversations in evidence.
With Mathematica’s expertise in rural health policy and data analytics, we equip states to move from uncertainty to sustainability.
Resources to Address Rising Costs
Rising healthcare costs make it critical for policymakers and program administrators to understand what’s driving spending growth and where to target improvements. Mathematica provides clarity through pricing and utilization data that make performance metrics easier to interpret and act on.
Our newly updated Rural Health Potentially Avoidable Utilization (PAU) Dashboard gives more than 1,600 rural hospitals nationwide insight into how PAU in emergency departments and inpatient settings impacts Medicare revenue—helping them identify where to invest to reduce potentially preventable, unplanned care.
We’ve also been a partner in developing resources such as a hospital cost tool and a health systems dashboard that provide policymakers and researchers with accessible data on hospital pricing, quality, and outcomes.
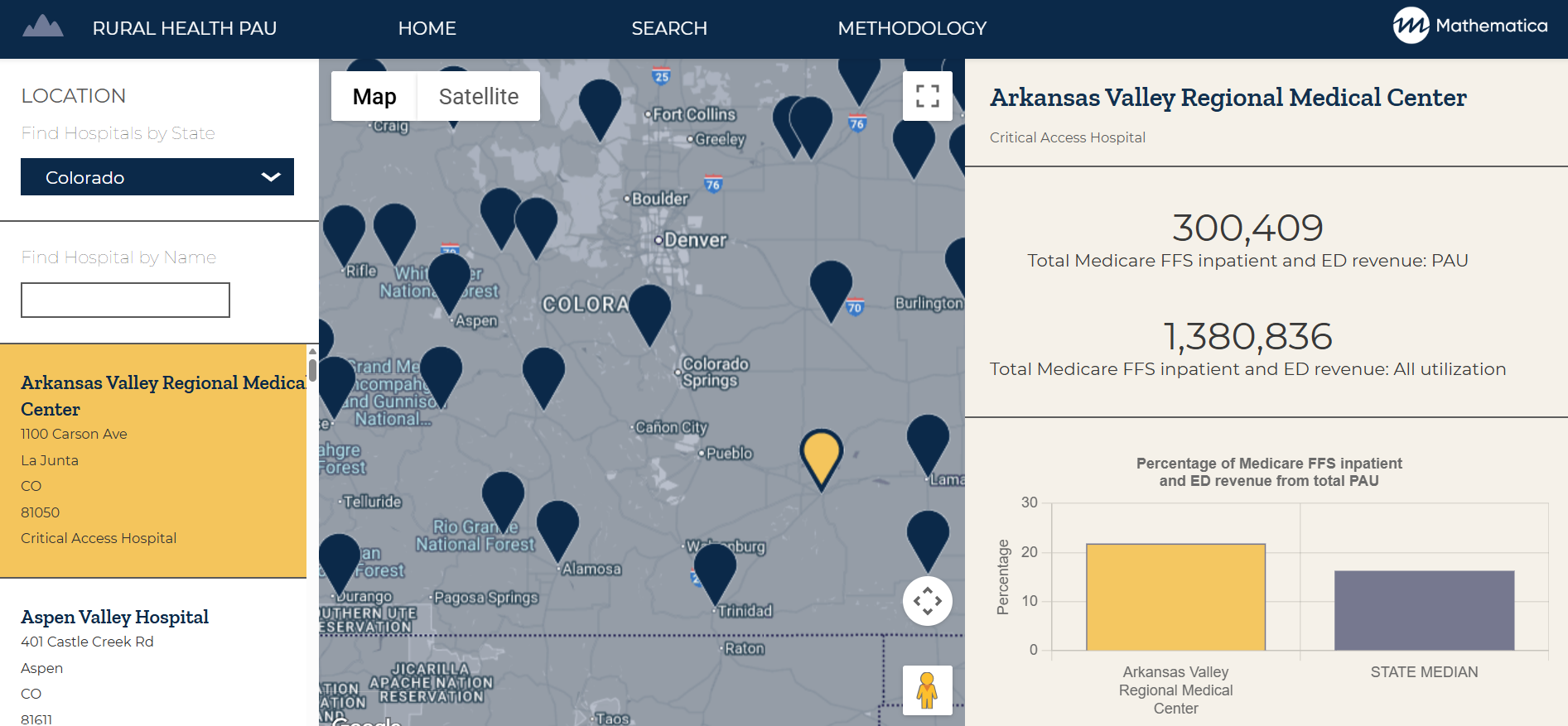
View Rural Hospital Data
Access potentially avoidable utilization rates by state for more than 1,600 rural hospitals using Mathematica’s updated interactive dashboard.
View DashboardEstablishing Rural Emergency Hospitals
Hospital closures continue to challenge rural communities, creating a shortage of accessible providers and forcing residents to travel long distances for essential care. To help sustain access, policymakers and CMS created the Rural Emergency Hospital (REH) designation—allowing communities that can’t support a full-service hospital to maintain 24-hour emergency, observation, and outpatient services.
Mathematica helps small rural hospitals, critical access hospitals, and rural community partners assess the feasibility and benefits of REH conversion. Through the REH Technical Assistance Center, we provide advisory services, financial modeling, virtual learning opportunities, and educational resources to guide hospitals through the transition process.

Supporting Small Rural Hospitals
Mathematica helps rural and critical access hospitals evaluate whether converting to a Rural Emergency Hospital is right for their community.
Learn MoreImplementing Alternative Payment Models
To curb rising costs and sustain rural healthcare, CMS and other payers are testing new approaches that reward care coordination, preventive care, and community health partnerships. These alternative payment models—including hospital global budgets—aim to stabilize financing while improving services for rural residents.
Mathematica supports states, federal agencies, payers, and providers in designing and implementing these models in rural settings with multi-payer participation, such as through our work on initiatives like the Vermont All-Payer ACO Model and the Pennsylvania Rural Health Model. We’ve partnered with the Pennsylvania Rural Health Redesign Center and the CMS Innovation Center to provide technical, financial, and data support that turns innovative payment models into practice.

Aligning Financial Incentives and Population Health
In Pennsylvania, global budget models helped hospitals cut Potentially Avoidable Utilization by focusing on better population health.
Learn MoreStrengthening Behavioral Health Services
Rural communities face unique challenges that heighten behavioral health needs—from provider shortages and geographic isolation to economic stress and limited access to broadband and transportation.
Mathematica works with governments, health systems, and community organizations to strengthen behavioral healthcare by identifying gaps in services, evaluating what works, and translating evidence into practical strategies for states and providers.
We analyzed a large health system in the Dakotas and rural Minnesota that integrated behavioral health into primary care—leading to improved quality-of-care processes and reduced emergency department use. We’ve also studied programs that support parents with substance use challenges who are involved in the child welfare system, helping identify strategies to promote recovery and family reunification. These insights guide the development of scalable, evidence-based solutions tailored to rural realities.

Working with Iowans to Strengthen Community-Based Services
We’re helping Iowa improve community-based services for Medicaid beneficiaries with health, disability, and aging needs.
Learn More



