As the U.S. continues to grapple with the COVID-19 pandemic and opioid epidemic, Mathematica experts are working with the Centers for Medicare & Medicaid Services (CMS) and states to help Medicaid and the Children’s Health Insurance Program (CHIP) better address the nation’s pressing health needs. At this year’s National Association of Medicaid Directors (NAMD) conference, held November 14–16, Mathematica experts will be available for scheduled meet and greets to discuss ways to address the opportunities and barriers facing state Medicaid programs as they transform care delivery and quality, modernize analytics and programs, and improve COVID-19 monitoring and after-action planning. Our experts look forward to meeting virtually and in person with state Medicaid directors at the NAMD fall conference to discuss how our expertise with data and technology can help states and CMS handle these new difficulties and opportunities.
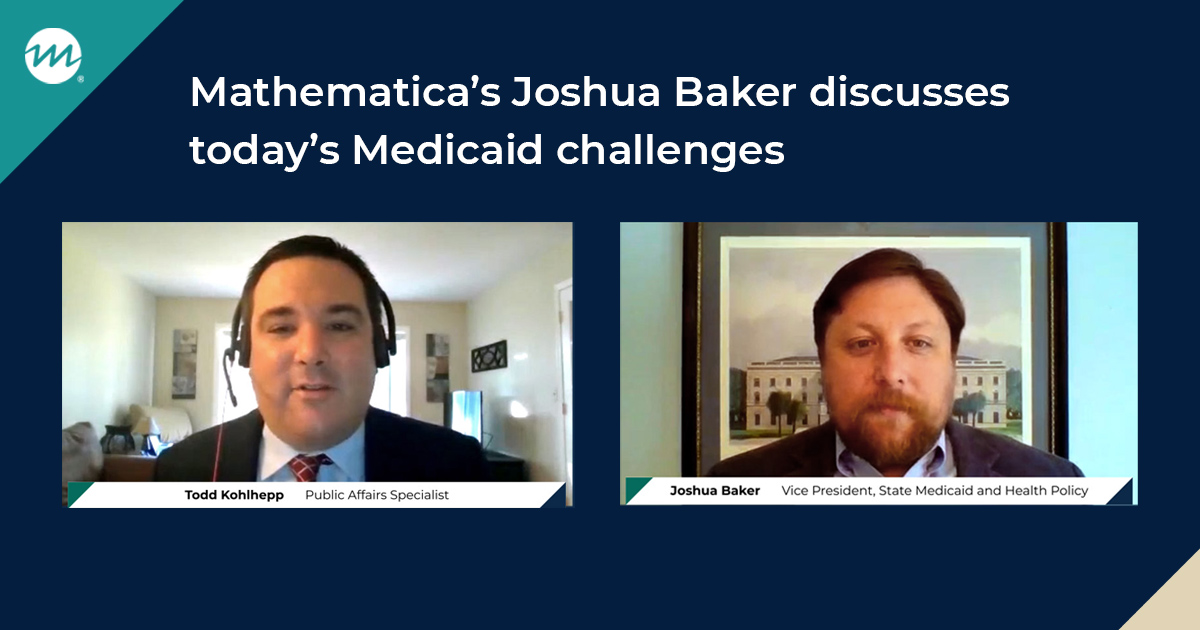
“State Medicaid programs and CMS face ongoing challenges in addressing COVID-19 and transitioning to value-based care. Digital solutions can provide timely insights to improve the delivery, quality, and affordability of health care provided to millions of Medicaid and CHIP beneficiaries, and we’re pleased to serve as collaborative partners in those efforts,” said Jonathan Morse, senior vice president and managing director of Health Program Improvement at Mathematica. “Our team, including Joshua Baker, former South Carolina Medicaid Director, has deep, first-hand experience with state Medicaid policies and programs, and we can co-create solutions that help fulfill the important missions of Medicaid agencies.”
Mathematica has recruited new staff and developed a suite of tools and technical assistance that can help states with diverse strategic, analytic, and operational needs:
Deliver strategic support across state Medicaid and health policy priorities
Contact Joshua Baker, vice president of Medicaid and state health policy, jbaker@mathematica-mpr.com
Joshua Baker was recently named vice president of state Medicaid and health policy at Mathematica. In this new position, he will lead state Medicaid and state health policy evaluation, analysis, and improvement, partnering with state health officials and agencies to improve access, quality, and cost. Learn more about Joshua Baker’s perspective on today’s Medicaid challenges.
Manage the COVID-19 pandemic and opioid epidemic and prepare for future public health crises
Mathematica is improving states’ ability to monitor the impacts of COVID-19 by using data from the Transformed Medicaid Statistical Information System (T-MSIS) to assess program outcomes. Our analysis of T-MSIS data is giving CMS timely information on how COVID-19 is affecting Medicaid and CHIP. We also developed the Substance Use Disorder (SUD) Data Book, which reports on the prevalence of SUD and opioid use disorder, categories of services provided by states, and use of services. As states wrestle with the COVID-19 and opioid epidemics, these kinds of data on peer state experiences can help drive continued innovation in Medicaid policy.
Apply Imersis: A digital solution to dive deep, explore, and refine T-MSIS data
Contact Paul Messino, senior researcher, pmessino@mathematica-mpr.com
Mathematica and NewWave teamed up to develop Imersis, a cloud-based data quality tool designed to help state Medicaid agencies prepare T-MSIS data for advanced analytics and meet new federal requirements. Mathematica has decades of experience reviewing and improving the quality of Medicaid data, and we have created online data tools in partnership with CMS, such as the DQ (Data Quality) Atlas, to give users accurate, extensive information on the quality of program data on enrollment, claims, expenditures, and service use. With Imersis, we bring this expertise to bear to help states get the most from their data systems.
Monitor the performance of long-term services and supports systems through integrated data analytics and measurement
Contact Jessica Ross, senior researcher, jross@mathematica-mpr.com
Mathematica helps states develop and deploy quality assurance and performance improvement systems for long-term services and supports (LTSS). Centralized management and analysis of diverse data sources make measurement possible across the continuum of key LTSS services and outcomes, including community integration and quality of life. We are also tracking the implications of the American Rescue Plan Act for home- and community-based services (HCBS), along with the need to monitor how new or enhanced services contribute to the goal of rebalancing states’ LTSS systems by increasing HCBS.
Support high-performing Medicaid managed care programs
Mathematica supports CMS in overseeing Medicaid managed care programs and helps states comply with federal Medicaid managed care requirements. We collect data on enrollment and other key features of these programs that help policymakers understand how managed care programs operate. We produce guidance for states on federal regulations and state best practices around special topics in managed care, such as provider network adequacy, access to behavioral health care, and encounter data validation. Our experts can also provide direct technical assistance to states.
Identify approaches to design, test, and scale new Medicaid policies
Contact Maggie Samra, senior director, msamra@mathematica-mpr.com
Mathematica works with states to develop data and reporting systems that can support innovative value-based care models, including reporting systems that engage participating providers in improving quality and managing costs. We have deep experience in both conducting 1115 demonstration evaluations and supporting CMS oversight of Medicaid 1115 demonstrations by developing tools and providing technical assistance to help CMS and states implement, monitor, and evaluate these policy experiments. Our team supports innovative demonstrations that address substance use disorder, serious mental illness/serious emotional disturbance, value-based care, and social determinants of health.
Measure the performance of Medicaid programs to increase transparency and drive improvement
Mathematica helps CMS develop the Medicaid and CHIP (MAC) Scorecard to increase public transparency about state programs and shed light on variation across states. States can access technical assistance from Mathematica to improve their use and understanding of the MAC Scorecard and jump-start program improvement in areas such as state and federal alignment, beneficiary health outcomes, and program administration.
Use quality measures to monitor and drive improvement in health outcomes
Mathematica draws on its expertise in health care quality measures to provide technical assistance and analytic support to CMS, states, and state quality partners (including managed care plans and providers), with the goal of improving the collection, reporting, and use of quality measures in Medicaid and CHIP. We also convene quality improvement learning collaboratives to help states and their quality partners improve performance in critical areas, including follow-up care for behavioral health, maternal and infant health, and health for foster care populations.