Policymakers have long pushed to shift the delivery of outpatient services away from hospital outpatient departments (HOPDs) to ambulatory surgical centers (ASCs) and physician offices, where costs are much lower. This past April, the Medicare Payment Advisory Commission (MedPAC) recommended that Congress impose site-neutral payments—meaning that Medicare would pay the same amount for outpatient services regardless of where the services are rendered. MedPAC estimated that the site-neutral payment policy would reduce Medicare payments and beneficiary cost sharing by $7.7 billion.
This recommendation prompted a few questions. To what extent do commercial health plans pay different prices for services delivered in different settings? Would health plans and consumers save money by choosing one setting over another for common services? For answers, we dug into our price transparency database, which collects, cleans, enriches, and analyzes vast volumes of pricing data released by commercial insurance plans under the federal Transparency in Coverage rules.
We first need to understand how Medicare pays for services in different care settings, as commercial plans mostly follow the same approach. For treatments provided in an HOPD or ASC, Medicare usually makes two payments—one to the facility for the cost of medical equipment, medical supplies, and overhead, and another to the doctor for the cost of professional work. The doctor fee is the same for ASCs and HOPDs, but the facility fee is generally lower for ASCs. As a result, the combined payment to an ASC would be lower than the payment for the same service at an HOPD.
For this case study, we picked Blue Cross Blue Shield of Texas’s Blue Choice preferred provider organization (PPO) plan, operated through one of the largest networks in Texas. We compared the prices for five ambulatory procedures commonly provided at both HOPDs and ASCs: colonoscopy with biopsy, cataract removal, hernia repair, knee arthroscopy, and ear tube insertion. Because the payer price data do not contain any provider information beyond their IDs, we used Mathematica proprietary data on provider identities to isolate hospital-based clinics and ASCs from freestanding physician group practices and individual clinicians. The outcome of interest is the total median price for each procedure, calculated by summing the median facility fee and median doctor fee of the procedure. The facility fee is reported in the payer price transparency data under the institutional class, whereas the doctor fee is reported under the professional class and might vary by place of service. Our analysis included 403 hospitals; 378 ASCs; and more than 100,000 physicians and clinicians in Texas.
Because of facilities fees, the same procedures cost more in HOPDs than in ASCs.
| Procedure (HCPCS code) | Setting | Facility price | Doctor price | Total price |
|---|---|---|---|---|
| Colonoscopy with biopsy (45380) | HOPD | $1,607 | $159 | $1,766 |
| ASC | $930 | $159 | $1,089 | |
| Cataract removal (66984) | HOPD | $3,235 | $493 | $3,727 |
| ASC | $1,917 | $493 | $2,410 | |
| Hernia repair (49505) | HOPD | $4,819 | $409 | $5,228 |
| ASC | $2,595 | $409 | $3,003 | |
| Knee arthroscopy (29881) | HOPD | $4,243 | $422 | $4,665 |
| ASC | $2,350 | $422 | $2,772 | |
| Ear tube insertion (69436) | HOPD | $2,140 | $122 | $2,262 |
| ASC | $1,101 | $122 | $1,223 |
Source: Mathematica’s payer price analytic database.
HCPCS = Healthcare Common Procedure Coding System.
HOPD = Hospital Outpatient Department.
ASC = Ambulatory Surgical Center.
For example, when a colonoscopy is provided in HOPDs, the median facility price is $1,607, compared with $930 at ASCs. The median doctor price is $159 for both HOPDs and ASCs. Combining facility and doctor fees, the total median price for a colonoscopy at HOPDs is $1,766, but it’s only $1,089 at ASCs—38 percent lower.
Across the five services we analyzed, the doctor prices do not differ between HOPDs and ASCs, but they are a small proportion of the total fee. Therefore, the differences in facility prices s between HOPDs and ASCs determine the differences in total prices.
Shifting care from HOPDs to ASCs would lead to considerable savings.
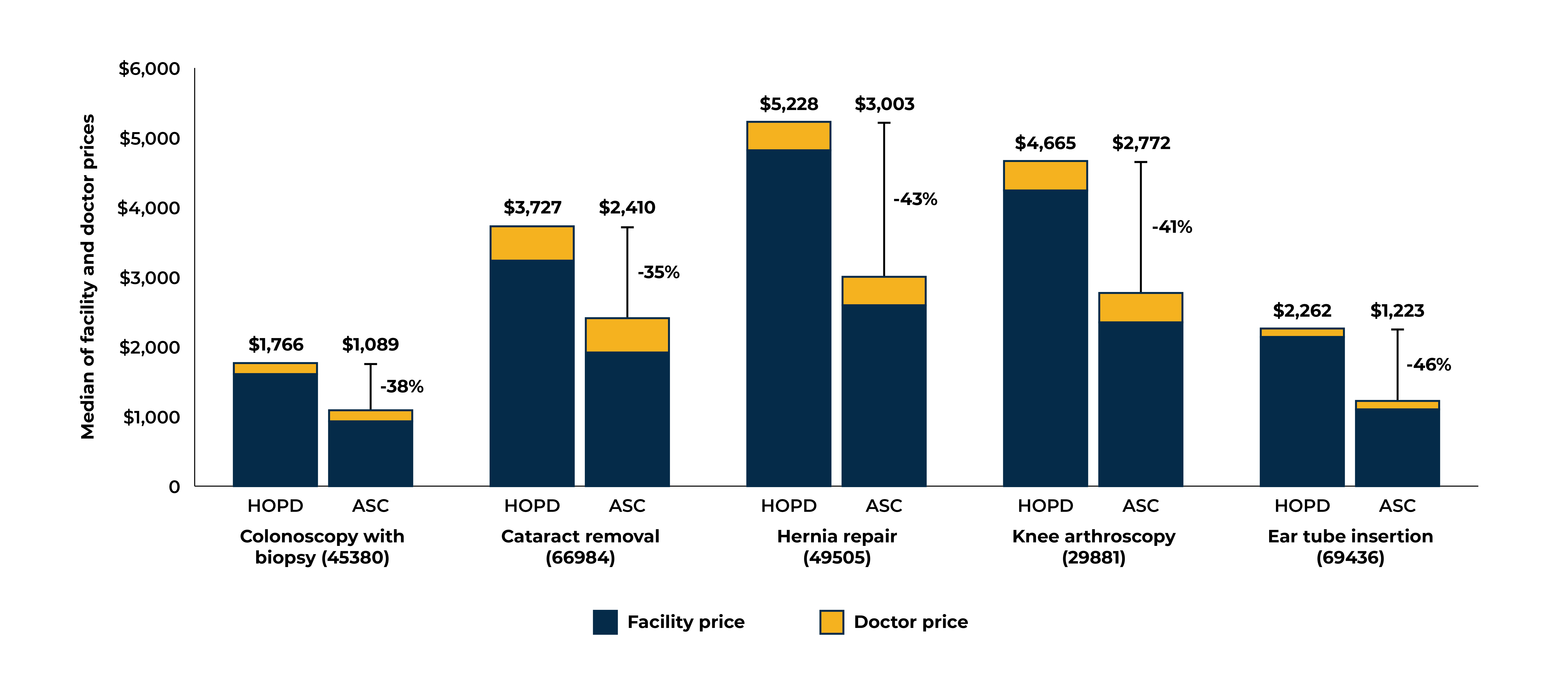
Source: Mathematica’s payer price analytic database.
HOPD = Hospital Outpatient Department.
ASC = Ambulatory Surgical Center.
Depending on the procedure, cost savings range from 35 percent for cataract removal to 46 percent for ear tube insertion per procedure. The aggregate cost savings could be significant for employers and employees. For example, about 4 million cataract procedures are performed in the U.S. each year. Assuming that each procedure at an HOPD costs $3,727, shifting 200,000 cataract removal procedures (5 percent of the total) would yield about $260 million in cost savings annually.
Prices also vary considerably across providers in each setting.
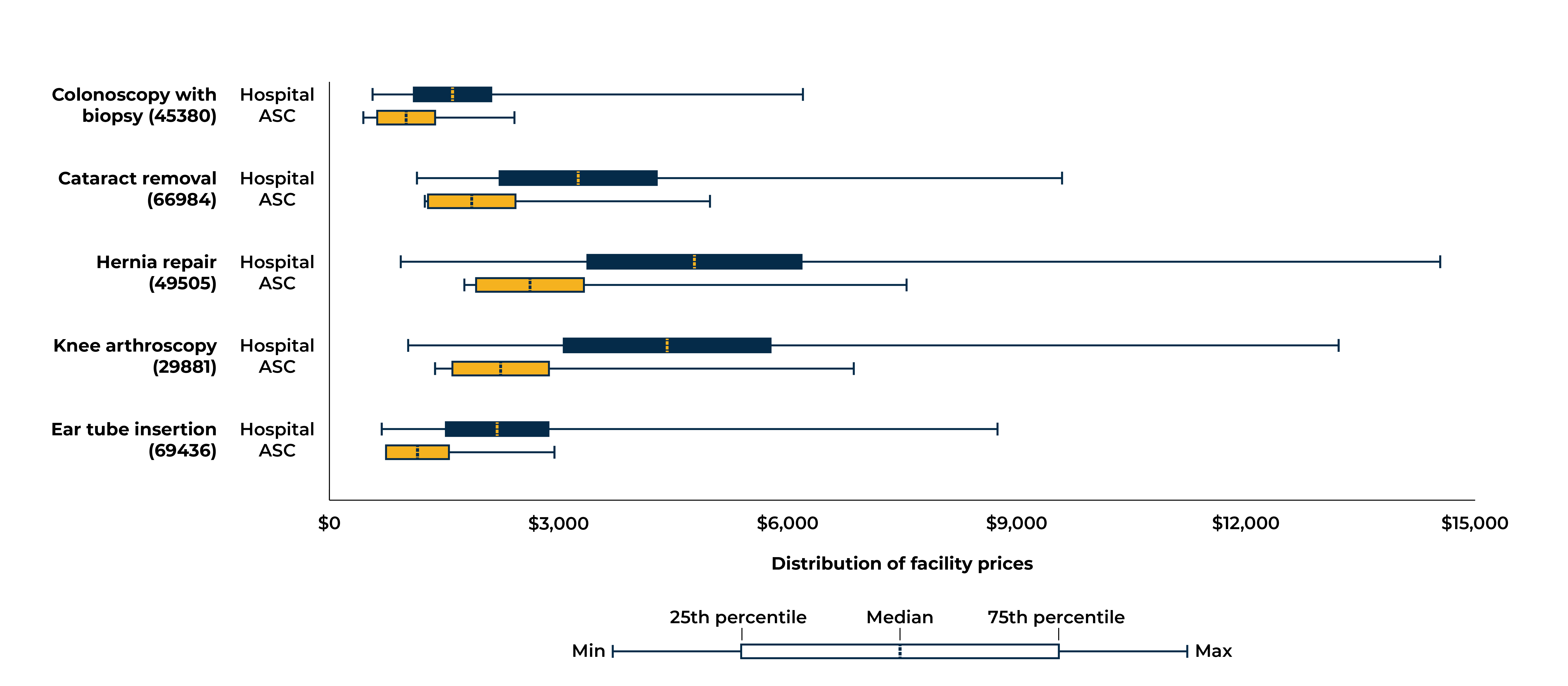
Source: Mathematica’s payer price analytic database.
HOPD = Hospital Outpatient Department.
ASC = Ambulatory Surgical Center.
For example, the boxplot for knee arthroscopy above shows that, in Texas, facility prices range from $1,018 to $13,226 (13 folds) among HOPDs and from $1,370 to $6,878 (5 folds) among ASCs. The boxplots also show that across procedures, the majority of ASCs have lower facility fees than HOPDs. For hernia repair and knee arthroscopy, even the price at the bottom quartile among HOPDs is higher than prices at the top quartile facility fee among ASCs.
Patients have an opportunity to demand better information from hospitals and health systems—and market innovators can help fill the gap.
Across the five procedures examined in our analysis, the plan-negotiated prices are considerably higher at hospitals than at ASCs. Although our analysis focused on just one plan in one state, our results are similar to results from a recent study of medical claims from a variety of commercial health plans. Sometimes the decision to go to hospital versus ASC depends on the complexity of the patient’s condition, but when options are available, patients should be aware of the cost differences between care settings when they decide where to receive treatment. However, few patients know about setting-based cost differences; even when they do, it is difficult to distinguish facility-based providers from office-based providers based solely on information available on the internet.
Developers of cost estimator tools can help close this information gap. The Transparency in Coverage final rules require that starting in 2023, health plans must provide real-time, personalized cost estimates to their members through an internet-based self-service tool. On the surface, such tools would empower consumers to seek care from lower-priced providers. But even though the professional costs are the same, the total cost of the treatment is likely higher in HOPDs than in ASCs when accounting for facility fees. For a cost estimation tool to be truly useful, it should include the estimated total cost of service depending on whether it is provided at a hospital facility, ASC, or freestanding office.
Price transparency data will help hospitals and health systems better prepare for payment policy changes.
Commercial payers have incentives that encourage lower health care costs by aligning payment rates across settings like Medicare does. As payment policies shift toward lower-cost settings, hospitals have less revenue to cover fixed costs to maintain emergency departments, standby capacity, and other hospital resources. The bottom-line impact of payment changes varies depends on multiple factors such as hospital payer mix, cost structure, patient population, and market structure. Using price transparency data to accurately anticipate these impacts will be key to better positioning hospitals and health systems for future changes in payment policies.
Visit Mathematica’s Health Care Price Transparency page for more information.