Project Overview
Mathematica developed two tools to shed light on the reasons for cost growth in Connecticut.
In the evolving landscape of health care spending, understanding the intricacies of health care cost growth has become increasingly vital. Mathematica has been working closely with states to implement benchmark programs for cost growth and to assess the drivers of this growth.
Connecticut Office of Health Strategy
In the evolving landscape of health care spending, understanding the intricacies of health care cost growth has become increasingly vital. Mathematica works closely with states to implement benchmark programs for cost growth and to assess the drivers of this growth.
Connecticut’s Office of Health Strategy (OHS) implemented the Healthcare Cost Growth Benchmark Program in January 2020 based on an executive order from Governor Ned Lamont. The purpose of the program is to benchmark growth in total health care expenditures in the state. From there, OHS established an annual growth rate for health care spending, making Connecticut the fifth state to have such a statewide benchmark, after Massachusetts, Delaware, Oregon, and Rhode Island.
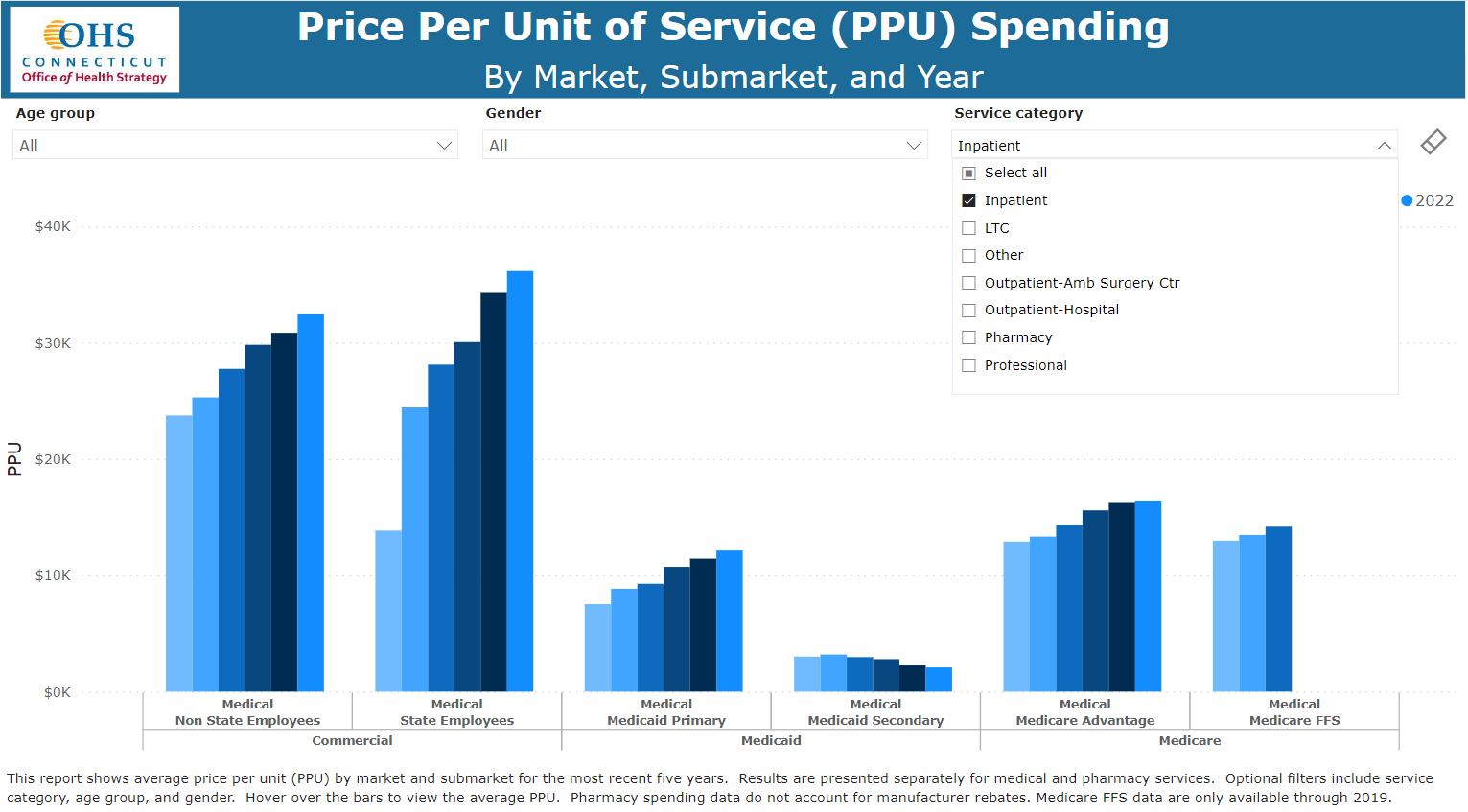
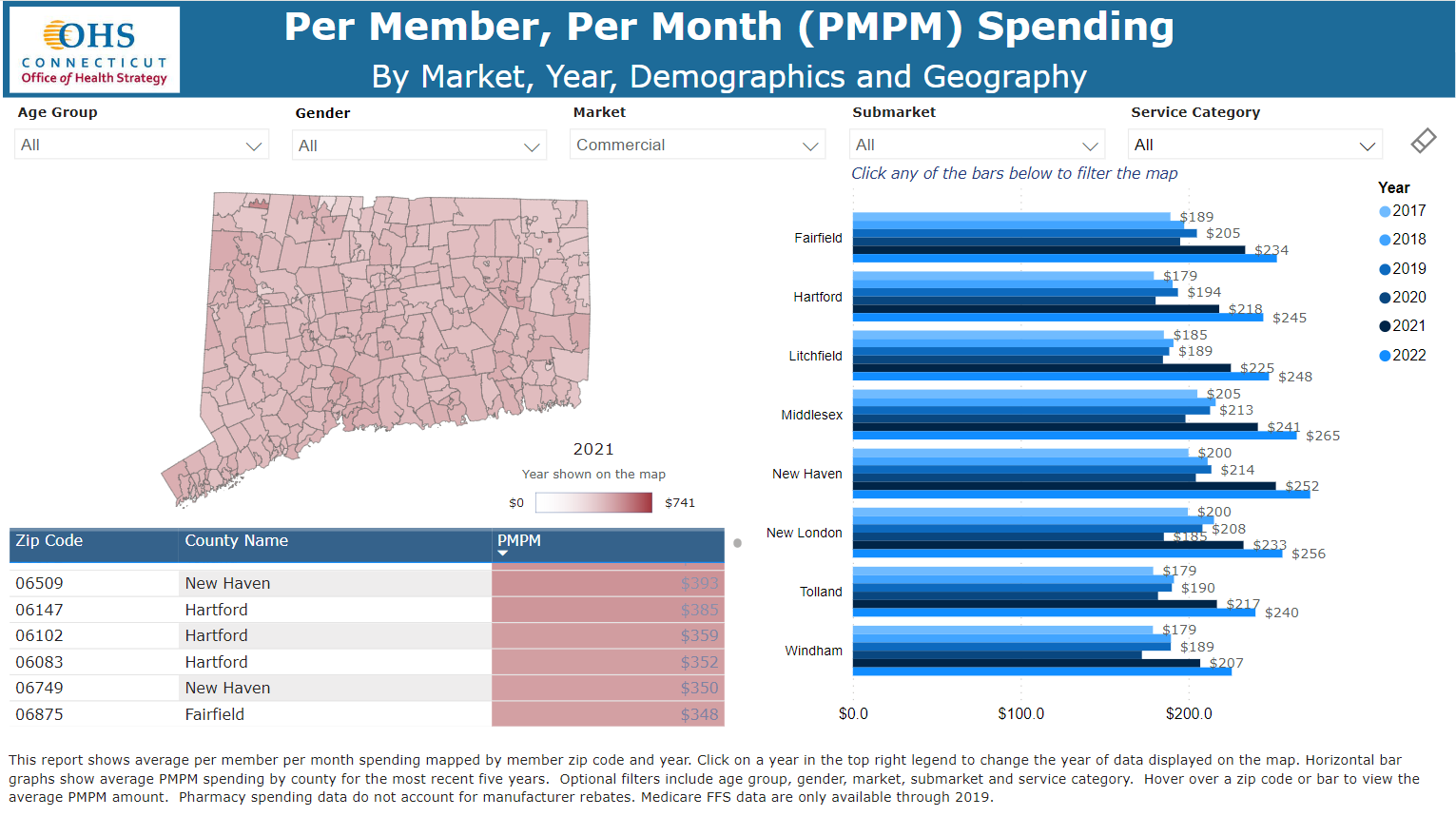
Supporting Connecticut, Mathematica created two tools to shed light on the drivers of cost growth in the state. The first is the Cost Driver Dashboard. This dashboard shows trends in health care spending over time at differing levels of granularity. Users can look at average spending per member per month, price per unit of service, volume of services, and trends in all of these measures from 2017 to 2022. Other functions enable users to visualize data by three types of insurance—commercial, Medicaid, and Medicare (Medicare fee-for-service data are available only through 2019)—and for inpatient, outpatient, long-term care, and other service categories. The dashboard also includes mapping of spending by zip codes across the state.
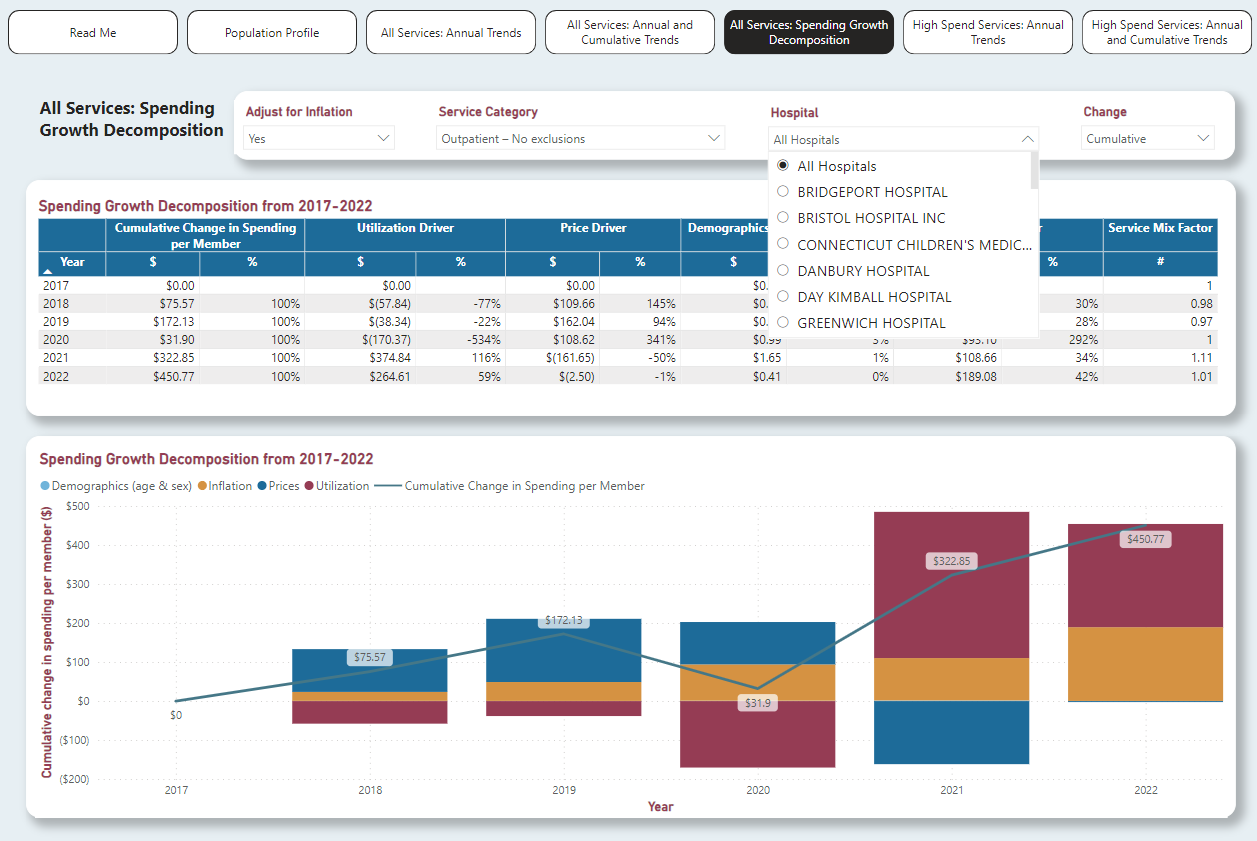
Hospitals are a main source of growth in health care costs. To help Connecticut identify the specific hospitals and hospital services driving growth, Mathematica also built the Hospital Cost Driver Dashboard. The dashboard disaggregates spending growth by price, volume, and demographics and enables users to filter to specific hospitals and hospital services. Both of these dashboards, developed in Power BI, are intended to help OHS identify where costs are rising fastest.
The Centers for Medicare & Medicaid Services (CMS) recently announced the States Advancing All-Payer Health Equity Approaches and Development (AHEAD) model, which focuses on slowing the growth of health care spending, improving health equity, and improving population health. Mathematica’s two new dashboards enable Connecticut and OHS to be more prepared to apply for the AHEAD model, as they will already have a tool to help pinpoint the drivers of rising costs. Along with Mathematica’s recently updated Potentially Avoidable Utilization Dashboard, dashboards like these can help states understand how they can best participate in CMS’s model.
Related Staff
Looking AHEAD: Partnering with States to Control Health Costs and Advance Health Equity
The Centers for Medicare & Medicaid Services’ States Advancing All-Payer Health Equity Approaches and Development (AHEAD) Model will provide selected states with funding to implement an alternative health care payment and service delivery model. Mathematica has extensive experience partnering with states and federal agencies, in addition to payer and provider communities, implementing state-based models similar to AHEAD.
Learn More



